Myth 1: If you have diverticular disease, you should avoid eating nuts, seeds and popcorn
Fact: This most persistent myth actually contradicts advice doctors give for preventing the condition in the first place. A healthy, high-fiber diet is actually the best medicine against diverticulitis, and seeds and nuts certainly fit the bill.
We used to think that a seed or nut plugged the pocket in the colon, and that’s what caused it to become inflamed or to rupture. But no surgeon has ever seen that, and studies have strongly suggested there’s nothing to that idea.
Myth 2: Diverticular disease always requires treatment
Fact: Patients often confuse the related conditions diverticulosis and diverticulitis.
Diverticulosis generally needs no treatment, while diverticulitis is a more serious condition that may require surgery.
Diverticulosis refers to small pockets that protrude through weak muscle layers in the intestinal wall, similar to a bubble in a tire. They’re fairly common. Sixty percent of people have them by age 60. Up to eighty percent of people have them by age 80.
A colonoscopy usually brings this condition to light, and it’s a very incidental finding. Most people don’t even realize they have the pockets, and by themselves, they are little cause for concern. Diverticulosis is like having freckles: It’s only a problem if those freckles turn into a mole. We don’t operate, ever, on diverticulosis.
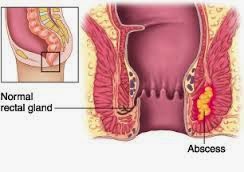
Diverticulitis occurs when one or more of those pockets are blocked by waste and inflammation or an infection occurs, or when pockets rupture and bacteria that are normally in your stool get outside of the intestines and into the surrounding abdominal area.
When this happens, a variety of complications can arise:
- You may experience pain and/or a fever.
- An abscess, or “walled-off” infection, may result from the bacteria in the abdomen.
- A painful infection of the abdominal cavity, or what we call peritonitis, occurs. Peritonitis is potentially fatal. Also, while it’s very uncommon, it does require immediate treatment.
Not everybody who has diverticulitis needs surgery, but they should see a physician, either in primary care or the emergency room, to get a proper diagnosis.
Myth 3: If you’ve had diverticulosis that developed into diverticulitis in the past, subsequent bouts of diverticulitis are more likely to perforate (and lead to peritonitis)
Fact: Diverticulitis happens in only 10 – 25 percent of those with diverticulosis. Also the great majority, or 75 percent, of those cases are the less serious type – requiring simple outpatient treatment, and perhaps medication.
Research shows the next bout of diverticulitis is most often going to be similar to your first bout. Usually, if your body could handle diverticulitis the first time, then the next time, it’s going to react just as well.
Lots of patients ask, “How do I prevent myself from getting diverticulitis?” Unfortunately, we don’t know why people get it. We think it’s from high pressure in the bowels and being constipated. We suggest eating a high-fiber, healthy diet and avoiding constipation.
Source: Cleveland Clinic