Tuesday 30 December 2014
Tuesday 16 December 2014
Scheduled for Surgery? How to Go In Strong, Ready
5 steps to improve surgery outcomes
If you are waiting to have a scheduled surgery, you may not realize that there are things you should do in those days or weeks before to increase your chances of a successful outcome.
 |
| Source: From internet |
Don’t simply wait for the scheduled date. Take these actions to be as healthy and strong as you can be, says general surgeon Kevin El-Hayek, MD. He offers patients these five tips:
1. Eat a “cleaner diet”
In the days before surgery, eat foods that are rich in vitamins and minerals. “I use the term, ‘cleaner diet,’ focused heavily on fruits and vegetables,” Dr. El-Hayek says. “We know that overall inflammation goes down when you eat foods rich in those respects.”
Also, avoid processed foods, red meat and other foods which are more difficult to break down. ”As the body is preparing for a shock that’s coming up, avoiding those things will decrease inflammatory markers,” he says.
2. Exercise regularly
Among other benefits, getting more exercise in the weeks before a surgery will increase your chances of walking sooner after the surgery.
“Even if you’re not an athlete, patients can train their bodies during the weeks leading up to surgery,” says Dr. El-Hayek. Even something as simple as parking farther away from the door where you work or shop can help.
“Shoot for 5,000 to 10,000 steps a day to increase your stamina. The main thing is that, undoubtedly, one of the discharge criteria you’re going to have to meet before you go home is getting close to your preoperative level of activity,” he says.
 |
| Source: From internet |
3. Kick bad habits
Use the time before surgery to quit smoking, stop drinking or using “any mood-altering substances that can affect your sleep or anxiety levels leading up to surgery,” Dr. El-Hayek says.
“Certainly in the few days leading up to surgery, alcohol and smoking can really affect the anesthesia.”
On the positive side, patients absolutely should engage in “meditation, prayer and things that are important to help people through the trauma that they’re about to undergo,” Dr. El-Hayek says.
 |
| Source: From internet |
4. See your internist
If you have two weeks or more before surgery, it’s especially important to check in and let your doctor know what’s coming up.
“Your primary doctor might want to make changes in your medications to optimize surgery,” Dr. El-Hayek says. “Your blood pressure and blood sugar need to be well-controlled. From a wound-healing standpoint, the better the sugars are controlled, especially for diabetics, the better recovery you’re going to have.”
And he mentions one other reason: “Your primary care physician is going to be the one who sees you afterward, who is going to be managing the changes that happen due to surgery.”
5. Find out about supplements, vitamins
Be sure to ask your doctor about vitamins and supplements, because some of them can interact with other medications, particularly anticoagulants.
Medications that impact bleeding, such as aspirin, anti-inflammatory drugs (like Advil®), Plavix® and Coumadin® probably should be stopped, Dr. El-Hayek says.
“But these questions are addressed in the pre-op medical clearance appointment,” he says. “It really is the provider’s role to counsel patients on medication/supplement usage as this varies from patient to patient.”
 |
| Source: From internet |
Source: Cleveland Clinic
Saturday 29 November 2014
Constipation: 6 Ways to Unblock Yourself
You’re bloated and blocked. You strain on the toilet with no results — or with results that are painful. You’re constipated.
Constipation is common. Sometimes it stems from stress. Other times it comes from bad diet or lifestyle choices. Still other times, it’s brought on by a medical condition that requires a doctor’s attention.
You can find relief, though, whether your constipation is a typical case or something more serious. The difference comes in how you find relief.
 |
| Pic from internet |
1. Solutions are simple for most people
Most of the time constipation happens because you’re not eating the right foods, you’re not drinking enough water and you’re not exercising enough. So the fixes are straightforward: Move more, drink more water and add fiber to your diet to add bulk to your stool. Some of the patients have had success taking probiotics, too, to change the composition of the bacteria in the gut.
 |
| Pic from internet |
2. Make time to move your bowels
This may sound simple, but people don’t always make bathroom time a priority. Try waking up earlier to eat breakfast and then move your bowels. Food can stimulate the need to go, and your home bathroom may be more relaxing. But don’t avoid public bathrooms when you feel the urge, either. Delaying a bowel movement can make constipation worse.
 |
| Pic from internet |
3. Look to your plate
Have you made a major change in your diet? Sometimes drastic changes to what you eat can cause constipation. For example, if you suddenly cut all fat from your diet, it’s easy to get blocked up. This can occur in weightlifters who eat all protein, no fat. It can happen in people with eating disorders, too. You don’t want to overdo fat, but you need a little to move things through your bowel.
4. When to see a doctor
Sometimes simple changes are not enough. If your constipation is more than just a short-term bother, if it’s not responding to treatments and if it lasts for weeks, get yourself checked out to exclude more serious medical causes. Chronic constipation can be a sign of conditions such as hyperthyroidism, hypercalcemia, celiac disease or irritable bowel syndrome (IBS). It’s especially important to see a professional if you have other symptoms such as dizziness, fatigue, cramping or spasms.
 |
| Pic from internet |
5. Fiber is not always the answer
Fiber works for most people, but not all. If fiber makes you more bloated and blocked than before, it could mean many different things. For example, in “slow transit constipation,” a condition where the bowel does not move things quickly through, fiber just sits there in your gut and can make you feel worse. Long story short: If fiber makes you worse, don’t just add more. Seek help.
6. If your constipation is serious, you have options
People with slow motility or IBS don’t have a cure for constipation, but you can treat it. There’s a wide range of laxatives available, plus pro-motility drugs that a doctor can prescribe. Sometimes at-home remedies can bring relief, too, including increasing dietary vegetable or mineral oil to lubricate the bowels. For people with celiac disease or wheat intolerance, cutting out gluten can make a world of difference.
Here’s the bottom line: Try simple fixes first, but if they fail, don’t suffer needlessly. See a doctor — and find out what treatments can get your bowels moving again.
Source: Cleveland Clinic
Sunday 16 November 2014
How You Can Deal With Anal Fissures
Anytime you have pain, bleeding and itching in your anal area, you’re going to worry.
First, these are all uncomfortable sensations — there’s no getting around that. And second, they can be scary and make you wonder, “What’s going on?”
Many patients will assume hemorrhoids are to blame, but there’s another common culprit behind symptoms such as these: anal fissures.
Anal fissures are small tears in the skin around your anus. They commonly cause itching and bleeding, and they tend to cause more pain than most types of hemorrhoids. When you have these symptoms, a doctor can help you get an accurate diagnosis — and the right kind of relief.
Risk factors — and how to lower them
Anal fissures can happen to just about anyone, but there are definitely factors that raise your risk. Constipation is a major one. Hard stool and straining on the toilet can put stress on your body and lead to these tears.
The same is true of diarrhea, even though it’s quite different from constipation. Anytime you have a change in your bowel habits that puts stress on your system, your risk goes up. That’s why we often see people come in with anal fissures after traveling, when changing diets put the digestive system to the test. Likewise, childbirth and the resulting stress on the body’s muscles and tissues can lead to fissures.
Fortunately, you can take preventive steps to lower your risk. They’re fairly simple:
- Drink plenty of water. Hydration helps you avoid constipation.
- Take an over-the-counter stool softener to avoid hard, dry bowel movements. Keeping things flowing through your body can help you avoid fissures. This is often good advice after childbirth in particular.
- Watch your diet, and make sure you’re getting plenty of fiber and leafy greens. For protein, choose lean meats and fish over red meat. And don’t eliminate all fat from your diet, because fat and oil are good lubricants that keep your digestive tract functioning properly.
What to do if you have a fissure
First, a doctor will want to rule out hemorrhoids or other conditions with similar symptoms, as well as abscesses, infections or other more serious concerns.
Next, in conjunction with the lifestyle changes outlined above, treatment for a fissure usually starts conservatively with simple at-home fixes and conservative medical therapy.
At home: A “sitz bath” — soaking in warm, but not hot, water several times a day — works wonders for many patients. The pain many people feel before or right after a bowel movement comes from muscle spasms brought on by the anal fissure. Warm baths help those muscles relax, which in turn helps the fissure heal over time.
Medical management: Medical therapy targets the muscles, too. A doctor may offer an ointment that relaxes the anal muscles so the fissure can heal, minus the spasms. A numbing agent such as lidocaine is an option, too, but I tend not to use it because it can add to the burning and irritation.
Surgical options: When conservative treatments don’t work, there are two simple outpatient surgical options. One is a Botox injection into the anal muscles. This basically paralyzes the muscle to prevent spasms and allow the fissure to heal. The other option is sphincterotomy, a strategic cut to the muscle that also relieves spasms. Both come with a healing time of around two weeks.
The best option comes down to your individual needs. For example, a sphincterotomy has a slight risk of causing long-term bowel control issues, so it is not recommended for people who already have those issues. The same is true of people with Crohn’s disease or HIV, two groups with an increased risk of anal fissures. For these populations, Botox may be a better option if surgery is required.
The bottom line — is that you have plenty of options to treat this irritating condition. When you suspect an anal fissure, see a doctor to confirm those suspicions and find out which options are best for you.
Source: Cleveland Clinic
Tuesday 4 November 2014
Your Colonoscopy: 7 Common Myths Debunked
Myth #1: “I’m not at risk for colon cancer.”
The truth is: Everyone is at risk, One in eighteen American men and women will get colon cancer in their lifetime. Adults above age 50 need to have a colonoscopy because the great majority of colorectal polyps – which are the precursors of colon cancer – occur after age 50. Removing polyps prevents colorectal cancer.
Myth #2: “If I don’t have any symptoms, I don’t need a colonoscopy.”
In nearly all cases, colon cancer starts as a precancerous growth in your colon, which usually doesn’t cause symptoms. A colonoscopy detects polyps so doctors can remove them before they turn into cancer. The idea is to do this before they cause symptoms. On average, endoscopists performing colonoscopies find precancerous polyps in 15 percent of women and 25 percent of men age 50 or over.
Myth #3: “There’s no way I can drink that prep stuff!”
Drinking a bowel preparation is one of the leading deterrents to having colonoscopy. The good news: Today’s bowel prep is easier than before. Rather than having to choke down a gallon of solution, patients can choose half-gallon options. What’s more, many physicians prescribe a split dose, where you take half the prep the night before and the other half on the morning of the procedure.
Myth #4: “A colonoscopy isn’t accurate.”
In 2008, a study reporting that colonoscopies may not completely protect against getting colon cancer gained a lot of media attention. But in that study, many colonoscopies were not complete and performed by general internists and family physicians who may not have had adequate experience to do the colonoscopy well.
More recent studies confirm that experience really matters when you choose who performs your colonoscopies. For a high quality colonoscopy, make sure your physician has specialized training in performing colonoscopies and tracks his or her outcomes as part of performance improvement.
Myth #5: “A colonoscopy is too painful!” or “I can’t be sedated enough.”
Actually, 99 percent of patients are adequately sedated through conscious sedation or twilight sleep and can be comfortable during their colonoscopy. Most patients don’t even remember the exam! Some hospitals also offer monitored anesthesia care for patients who require deeper sedation.
Myth #6: “It’s too risky. My friend had his colon perforated during a colonoscopy.”
When performed by specially trained professionals, colonoscopies are extremely safe. The risk of perforation is less than 1 in 1,000 cases, and the risk of bleeding is less than 1 percent.
Myth #7: “If I get colorectal cancer, then it was meant to be.”
Not true. Colon cancer is preventable. Here’s how: Begin screening for colon cancer (colonoscopy is the preferred screening strategy) at age 50, or earlier if you have risk factors. Other things you can do: Improve your diet, maintain a normal body weight, exercise and avoid smoking.
Source: Cleveland Clinic
Friday 24 October 2014
Diverticular Disease: Greatest Myths and Facts
Myth 1: If you have diverticular disease, you should avoid eating nuts, seeds and popcorn
Fact: This most persistent myth actually contradicts advice doctors give for preventing the condition in the first place. A healthy, high-fiber diet is actually the best medicine against diverticulitis, and seeds and nuts certainly fit the bill.
We used to think that a seed or nut plugged the pocket in the colon, and that’s what caused it to become inflamed or to rupture. But no surgeon has ever seen that, and studies have strongly suggested there’s nothing to that idea.
Myth 2: Diverticular disease always requires treatment
Fact: Patients often confuse the related conditions diverticulosis and diverticulitis.
Diverticulosis generally needs no treatment, while diverticulitis is a more serious condition that may require surgery.
Diverticulosis refers to small pockets that protrude through weak muscle layers in the intestinal wall, similar to a bubble in a tire. They’re fairly common. Sixty percent of people have them by age 60. Up to eighty percent of people have them by age 80.
A colonoscopy usually brings this condition to light, and it’s a very incidental finding. Most people don’t even realize they have the pockets, and by themselves, they are little cause for concern. Diverticulosis is like having freckles: It’s only a problem if those freckles turn into a mole. We don’t operate, ever, on diverticulosis.
Diverticulitis occurs when one or more of those pockets are blocked by waste and inflammation or an infection occurs, or when pockets rupture and bacteria that are normally in your stool get outside of the intestines and into the surrounding abdominal area.
When this happens, a variety of complications can arise:
- You may experience pain and/or a fever.
- An abscess, or “walled-off” infection, may result from the bacteria in the abdomen.
- A painful infection of the abdominal cavity, or what we call peritonitis, occurs. Peritonitis is potentially fatal. Also, while it’s very uncommon, it does require immediate treatment.
Not everybody who has diverticulitis needs surgery, but they should see a physician, either in primary care or the emergency room, to get a proper diagnosis.
Myth 3: If you’ve had diverticulosis that developed into diverticulitis in the past, subsequent bouts of diverticulitis are more likely to perforate (and lead to peritonitis)
Fact: Diverticulitis happens in only 10 – 25 percent of those with diverticulosis. Also the great majority, or 75 percent, of those cases are the less serious type – requiring simple outpatient treatment, and perhaps medication.
Research shows the next bout of diverticulitis is most often going to be similar to your first bout. Usually, if your body could handle diverticulitis the first time, then the next time, it’s going to react just as well.
Lots of patients ask, “How do I prevent myself from getting diverticulitis?” Unfortunately, we don’t know why people get it. We think it’s from high pressure in the bowels and being constipated. We suggest eating a high-fiber, healthy diet and avoiding constipation.
Source: Cleveland Clinic
Monday 20 October 2014
5 Facts You Should Know About Your Poops
There is no normal
People are different. So are bowel movements. The size, shape and consistency of feces will change greatly from person to person.
Instead of looking for “normal,” look for a change. Did you use to move your bowels frequently but now have trouble doing so? Did they use to be solid but now are runny for a long period of time? When you experience a big, noticeable change that lasts, it’s time to see your doctor.
Blood is a warning sign
If there is blood in your feces on a recurring basis, see a doctor. Blood can be a sign of polyps or colorectal cancer. It also can be caused by benign conditions such as hemorrhoids and anal fissures. In any case, it’s worth getting checked out.
If you see blood, keep an eye out for other symptoms: weight loss, fever, chills. When they come together, those are “high-alert” symptoms of bowel disorders.
Sometimes size is a concern
If you used to have sizeable stools but now they are always pencil thin and hard to pass, consult your doctor. In certain types of colon cancer, the bowel gets narrow, and so do your bowel movements.
Thin stools do not automatically mean cancer. But if they last a long time and if going to the bathroom is difficult for you, your doctor may order a colonoscopy to rule it out.
Consistency matters
We all have bouts of diarrhea from time to time. Runny, watery stool over a short period of time can mean mild food poisoning or an infection, for example.
But if you used to have solid bowel movements and now have diarrhea frequently, it could be a sign of an inflammatory bowel disease such as Crohn’s disease or ulcerative colitis — especially if it comes with other symptoms such as abdominal pain, blood and weight loss.
It could be stress
Your body reacts to things that go on around us. The impact of stress and unresolved issues may show up in your bathroom.
Your bowels may be indicating something that you’re not appreciating consciously. If your bathroom habits have changed drastically and other medical causes have been excluded, life’s stresses may be to blame.
Pay attention to what your bowels are telling you. From stress to medical conditions, they may give you warning sings that will help you improve your health.
Source: Dr Brooke Gurland, MD, Cleveland Clinic
Monday 13 October 2014
Things You Need To Know About Fistula-in-ano
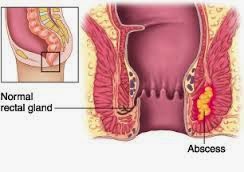
What Is An Anal Abscess?
An anal abscess is an infected cavity filled with pus found near the anus or rectum.What Is An Anal Fistula (Fistula-in-ano)?
An anal fistula is frequently the result of a previous or current anal abscess. The small glands just inside the anus occasionally get clogged and potentially can become infected, leading to an abscess. The fistula is a tunnel that form under the skin and connects the infected glands to the abscess. A fistula can present with or without and abscess and may connect just to the skin of the buttocks near the anal opening. Other causes of fistula include Crohn's disease, tuberculosis, radiation, trauma and malignancy.How Does Someone Get An Anal Abscess Or A Fistula?
The abscess is most often a result of an acute infection in the internal glands of the anus. Occasionally, bacteria, faecal material or foreign matter can clog the gland and create a condition for an abscess cavity to form.After an abscess drains on its own or has been drained (opened), a tunnel (fistula) may persist connecting the infected anal gland to the external skin. This typically will involve some type of drainage from the external opening and occurs in up to 50% of the abscesses. If the opening on the skin heals when the fistula is present, a recurrent abscess may develop.
What Are The Signs And Symptoms Of An Abscess Or Fistula?
A patient with an abscess may have pain, redness or swelling around the anal area. Fever or chills are also common. In a patient with a fistula, there will be additional symptoms of irritation of the perianal skin or drainage from an external opening.Is Any Specific Testing Necessary To Diagnose An Abscess Of Fistula?
No. Most of the abscesses or fistula are diagnosed and managed on the basis of clinical findings. Occasionally, a MRI or endoanal ultrasound can assist with the diagnosis of deeper abscesses or the delineation of the fistula tunnel to help guide treatment.What Is The Treatment Of An Anal Abscess?
Surgical drainage is needed under most circumstances. An incision is made in the skin near the anus to drain the pus. It can be performed under local anaesthesia or general anaesthesia for bigger and deeper abscess. The wound would be left open and let it heal by itself. Hospitalisation may be required in patients prone to more significant infections such as diabetics or patients with decreased immunity.What Is The Treatment Of An Anal Fistula?
Surgery is almost always necessary to cure an anal fistula. Although surgery can be fairly straightforward, it may also be complicated, occasionally requiring staged or multiple operations. It is advisable to consult a colorectal surgeon to discuss the different types of potential operations.The surgery may be performed at the same time as drainage of an abscess, although sometimes the fistula does not appear until weeks to years after the initial drainage. If the fistula is straightforward, a fistulotomy may be performed. Other procedures include placing material within the fistula tract to occlude it or surgically altering the surrounding tissue to accomplish closure of the fistula, with the choice of procedure depending upon the type, length and location of the fistula.
What Is The Recovery Like From Surgery?
Pain after surgery is controlled with painkillers, fibers and bulk laxatives. Sitz bath is encouraged and to avoid constipation. You can discuss with your surgeon the specific care and time away from work prior to surgery to prepare yourself for post-operative care.Can The Abscess Or Fistula Recur?
Yes. Both abscesses and fistulas can potentially recur. Should similar symptoms arise, suggesting recurrence, it is recommended that you visit a colorectal surgeon to manage your condition.
Source:ASCRS
Friday 19 September 2014
Things You Need To Know About Anal Fissure
What Is An Anal Fissure?
An anal fissure is a small, oval-shaped tear in skin that lines the opening of the anus. It causes severe pain and bleeding during bowel movements. It is quite common, but often confused with other causes of pain and bleeding, such as haemorrhoids.What Are The Symptoms of Anal Fissure?
The symptoms include severe pain during, and especially after a bowel movement, lasting from several minutes to a few hours. There might be bright red blood from the anus that can be seen on toilet paper or on the stool. Between bowel movements, patients with anal fissures are often symptom-free. They are fearful of having a bowel movement and may try to avoid defecation due to the pain.What Causes Anal Fissure?
They are usually caused by trauma to the inner lining of the anus. Patients with tight anal sphincter muscles (i.e. increased muscle tone) are more prone to developing anal fissures. A hard, dry stool is typically responsible; but loose stools and diarrhoea can also be the cause.Following a bowel movement, severe anal pain can produce spasm of the anal sphincter muscle, resulting in a decrease in blood flow, thus impaired healing of the wound. The next bowel movement results in more pain, anal spasm, decrease blood flow to the area, and the cycle continues. Treatments are aimed at interrupting this cycle by relaxing the anal sphincter muscle to promote healing of the fissure.
Other less common causes include inflammatory conditions and certain anal infections or tumours. Anal fissures may be acute (recent onset) or chronic (present for a long period of time). Chronic fissures may be more difficult to treat, and usually will have an external lump (sentinel pile or skin tag).
What Is The Treatment Of Anal Fissures?
Majority do not require surgery. The treatment of acute fissure consists of high fiber diet, increased water intake and stool softeners. Topical anaesthetics for pain and warm sitz baths for 10-20 minutes several times a day (after bowel movements) are soothing and promote relaxation of anal muscles.Other medications (nitroglycerin, nifedipine, diltiazem cream) can be prescribed to allow relaxation of the anal sphincters. Chronic fissures are generally more difficult to treat and may need surgical treatment.
Will The Problem Return?
Yes. It is quite common for a fully healed fissure to recur after a hard bowel movement or other trauma. It is very important to continue good bowel habits and a diet high in fiber as a lifestyle change. If the problem returns without an obvious cause, further assessment is warranted.What Does Surgery Involve?
Surgical options include Botox injection into the anal sphincter and surgical division of a portion of the internal anal sphincter (lateral internal sphincterotomy). Both of these procedures can be performed as outpatient, same-day procedures. The goal of these surgical options is to promote relaxation of the anal sphincter, thereby reducing anal pain and spasm, allowing the fissures to heal. Botox injection results in healing in 50-80% of patients while sphincterotomy is reported to be >90% successful. All surgical procedures carry some risk; and your colorectal surgeon will discuss these risks with you to determine the appropriate treatment for your particular situation.How Long Is The Recovery After Surgery?
Complete healing can take up to 6-10 weeks. However, acute pain after surgery often disappears after a few days. Most patients will be able to return to work and resume daily activities in a few short days after surgery.Can Fissure Lead to Colon Cancer?
Absolutely NO. Persistent symptoms, however, need careful evaluation since other conditions can cause similar symptoms. A colonoscopy may be required to exclude other causes of rectal bleeding.
Source: ASCRS
Sunday 7 September 2014
Things You Need To Know About Diverticular Disease
What Is Diverticulosis/Diverticulitis?
Diverticula are pockets that develop in the colon wall, usually in the sigmoid or left colon, but may involve the entire colon.
Diverticulosis means the presence of these pockets. Diverticulitis are inflammation or complications of these pockets.
What are the Symptoms of Diverticular Disease?
Uncomplicated diverticular disease is usually not associated with symptoms. Symptoms are related to complications of diverticular disease including diverticulitis and bleeding. Diverticular disease is a common cause of significant bleeding from the colon.
Diverticulitis - an infection of the diverticula. It may cause one or more of the following symptoms:
- Pain in the abdomen
- Chills, fever
- Change in bowel habits
More intense symptoms are associated with serious complications such as perforation (rupture), abscess or fistula formation (an abnormal connection between the colon and another organ or the skin).
What is the Cause of Diverticular Disease?
The cause is not precisely known, but it is more common for people with a low fiber diet. It is thought that a low-fiber diet over the years creates increased colon pressure and results in pockets or diverticula.
How Is Diverticular Disease Treated?
Increasing the amount of dietary fiber (grains, legumes, vegetables, etc.) - and sometimes restricting certain food reduces the pressure in the colon and may decrease the risk of complications due to diverticular disease.
Diverticulitis requires different management. Mild cases may be managed with antibiotics, dietary restrictions and possibly stool softeners. More severe cases require hospitalisation with intravenous antibiotics and dietary restrains. Most acute attacks can be relieved with such methods.
When Is Surgery Necessary?
Surgery is reserved for patients with recurrent episodes of diverticulitis, complications or severe attacks when there is no response to medication. Surgery may also be required in individuals with bleeding from diverticulosis.Surgery is also needed if patients developed complications from diverticulitis (stricture, obstruction, fistula).
Surgical treatment for diverticulitis removed the diseased part of colon. Complete recovery can be expected. In emergency surgeries, patients may require a temporary colostomy bag. Patients are encouraged to seek medical attention for abdominal symptoms early to help avoid complications.
Diverticula are pockets that develop in the colon wall, usually in the sigmoid or left colon, but may involve the entire colon.
Diverticulosis means the presence of these pockets. Diverticulitis are inflammation or complications of these pockets.
What are the Symptoms of Diverticular Disease?
Uncomplicated diverticular disease is usually not associated with symptoms. Symptoms are related to complications of diverticular disease including diverticulitis and bleeding. Diverticular disease is a common cause of significant bleeding from the colon.
Diverticulitis - an infection of the diverticula. It may cause one or more of the following symptoms:
- Pain in the abdomen
- Chills, fever
- Change in bowel habits
More intense symptoms are associated with serious complications such as perforation (rupture), abscess or fistula formation (an abnormal connection between the colon and another organ or the skin).
What is the Cause of Diverticular Disease?
The cause is not precisely known, but it is more common for people with a low fiber diet. It is thought that a low-fiber diet over the years creates increased colon pressure and results in pockets or diverticula.
How Is Diverticular Disease Treated?
Increasing the amount of dietary fiber (grains, legumes, vegetables, etc.) - and sometimes restricting certain food reduces the pressure in the colon and may decrease the risk of complications due to diverticular disease.
Diverticulitis requires different management. Mild cases may be managed with antibiotics, dietary restrictions and possibly stool softeners. More severe cases require hospitalisation with intravenous antibiotics and dietary restrains. Most acute attacks can be relieved with such methods.
When Is Surgery Necessary?
Surgery is reserved for patients with recurrent episodes of diverticulitis, complications or severe attacks when there is no response to medication. Surgery may also be required in individuals with bleeding from diverticulosis.Surgery is also needed if patients developed complications from diverticulitis (stricture, obstruction, fistula).
Surgical treatment for diverticulitis removed the diseased part of colon. Complete recovery can be expected. In emergency surgeries, patients may require a temporary colostomy bag. Patients are encouraged to seek medical attention for abdominal symptoms early to help avoid complications.
Source: ASCRS
Saturday 30 August 2014
Four simple ways to prevent Hemorrhoids
1. Go when you need to go
This sounds like common-sense advice, but too many people ignore it. If you delay using the bathroom, your stool may become hard and dry in your bowel, which makes it harder to pass. If you strain to pass stool, your risk for hemorrhoids rises.
Speaking of straining, don’t force a bowel movement when you don’t need to go, either. Straining increases the pressure on your venous cushions, which leads to hemorrhoids. In particular, straining can turn internal hemorrhoids into external ones.
2. Don’t turn the bathroom into a library
Think of your time in the bathroom as a necessity, not an extended escape. If your toilet has stacks of magazines or books on the water tank, consider moving them to another room.
Why? The more time you spend on the toilet, the more likely you will strain for bowel movements. Also, the seated position puts extra stress on your anal blood vessels. Both of these factors boost your risk of haemorrhoids.
3. Reassess your diet
To prevent hemorrhoids, you want stool that is soft and easy to pass. You can reach the right consistency by making smart diet choices and drinking plenty of water to avoid dehydration. lack of fiber is the most common culprit. For example, if you find yourself constipated, try getting more fiber from green vegetables and100 percent whole grains. If need be, ask your doctor about taking fiber supplements, but start by trying to get fiber through your diet. Fiber can help you avoid constipation, and constipation — which leads to straining — is a risk factor for hemorrhoids.
Fiber comes with a warning, though. Some people have what we call “slow transit constipation.” Their bowels move slower than normal. For these people, excess fiber tends to sit in the gut and make constipation worse.
Also, listen to your body and avoid foods that irritate your bowels. For some people, the lactose in dairy products is an irritant. For others, it’s gluten or too many refined foods.
4. Get moving
Exercise helps improve or prevent many bowel and digestive issues, including hemorrhoids. When you are sedentary, everything slows down, including your bowels.
Exercise helps keep waste moving through your intestinal tract. In turn, this helps you avoid constipation and dry, hard stool. Walking, running, biking, yoga — take your pick, but choose an active lifestyle.
One note of caution, though: Avoid heavy-duty weight-lifting squats and similar motions that increase abdominal pressure. If you’re trying to prevent hemorrhoids, these exercises can do more harm than good.
Source: Cleveland Clinic
Subscribe to:
Posts (Atom)